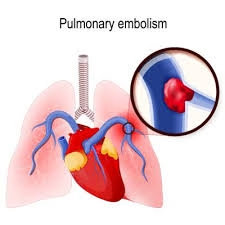
Pulmonary Embolism is a high risk acute chest condition that quickly escalate into RV failure , circulatory collapse and death. Today we cover a diagnostic roadmap to tackle such a condition in the ER
1. Overview
Pulmonary embolism is a blockage of the pulmonary arteries, usually by a thrombus that originated in the deep veins of the legs (DVT). It’s a spectrum — from incidental small emboli to life-threatening massive PE causing shock.
2. Clinical Picture
PE often presents nonspecifically, so a high index of suspicion is crucial.
Common symptoms:
- Sudden dyspnea (most common)
- Pleuritic chest pain
- Cough ± hemoptysis
- Syncope (suggests massive PE)
Signs:
- Tachypnea, tachycardia
- Hypoxia (low O₂ saturation)
- Hypotension, raised JVP, RV gallop → massive PE
- Signs of DVT (leg swelling, tenderness) in ~30–50%
Severity stratification (ESC):
- Massive / High-risk PE: Hemodynamic instability (SBP < 90 mmHg or shock)
- Submassive / Intermediate-risk: Stable BP but RV dysfunction or elevated troponin/BNP
- Low-risk: Hemodynamically stable, no RV dysfunction or biomarker rise
3. Investigations & Diagnosis
Step 1: Assess Clinical Probability
Use Wells score or revised Geneva score.
Example (simplified Wells):
- DVT signs → +3
- PE most likely → +3
- HR > 100 → +1.5
- Immobilization / surgery → +1.5
- Previous DVT/PE → +1.5
- Hemoptysis → +1
- Malignancy → +1
Interpretation:
- ≤4: PE unlikely
- 4: PE likely
Step 2: D-dimer
- If low/intermediate probability, order D-dimer.
- Negative D-dimer effectively rules out PE.
- Age-adjusted cutoff = (age × 10 µg/L) for patients >50.
- If high clinical probability, skip D-dimer and go straight to imaging.
Keep in mind a D-Dimer test could actually turn out negative in a PE case ,although rare, therefore when clinical suspicion is paramount , we skip it
Step 3: Imaging
- CT Pulmonary Angiography (CTPA) → gold standard for diagnosis.
- Confirms embolus in main/lobar/segmental arteries.
- V/Q scan → alternative if CTPA contraindicated (e.g., renal failure, contrast allergy).
- Lower limb Doppler → if PE suspected but imaging unavailable, can indirectly support diagnosis.
Step 4: Supporting tests
- ABG: Often shows hypoxia + respiratory alkalosis (not diagnostic).
- ECG: Sinus tachycardia, S1Q3T3 pattern, RBBB, T-wave inversions V1–V4.
- Echocardiography: Assesses RV strain — crucial in unstable patients.
- Cardiac biomarkers: Elevated troponin or BNP → RV dysfunction → worse prognosis.
4. Diagnosis (Summary Criteria)
✅ Confirmed PE =
- Objective imaging evidence (CTPA or V/Q) of intraluminal filling defect, OR
- Positive DVT imaging in a symptomatic patient with clinical suspicion of PE.
Other Articles :
Med Bites : Unstable Angina , NSTEMI , STEMI