Overview
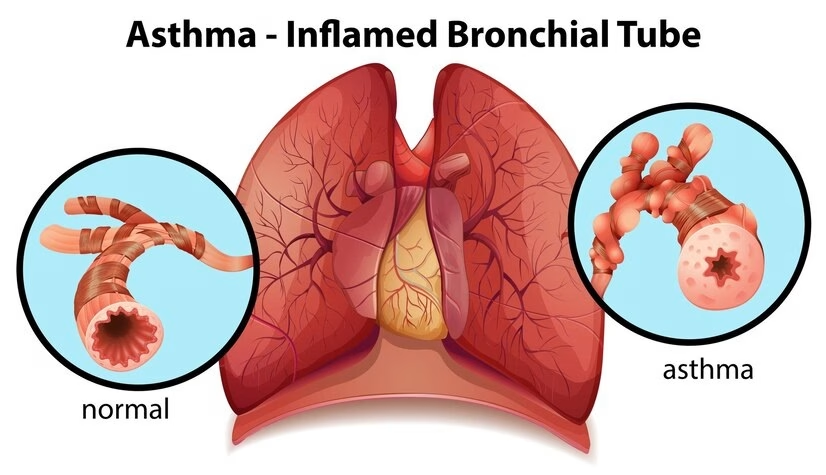
Bronchial asthma is a chronic inflammatory disorder of the airways that causes reversible airflow obstruction and airway hyperresponsiveness. It’s characterized by episodes of wheezing, cough, chest tightness, and shortness of breath, often triggered by allergens, exercise, infections, or environmental factors.
Clinical Picture
- Symptoms:
- Episodic wheezing, shortness of breath, chest tightness, and cough (especially at night or early morning).
- Symptoms often vary over time and worsen with triggers like cold air, dust, smoke, exercise, or viral infections.
- Signs (during an attack):
- Prolonged expiration, diffuse wheezing on auscultation.
- Tachypnea, tachycardia, use of accessory muscles in severe attacks.
- Between attacks: patient may be asymptomatic with a normal exam.
Diagnosis and Investigations
Diagnosis is based on clinical features plus objective evidence of reversible airflow limitation.
1. Pulmonary Function Tests (Spirometry):
- ↓ FEV₁/FVC ratio (<0.75–0.8)
- Significant reversibility after bronchodilator (↑FEV₁ ≥12% and ≥200 mL).
- Peak expiratory flow (PEF) variability >20% supports diagnosis.
2. Additional Tests (if uncertain):
- Bronchial provocation test (e.g., methacholine challenge) – positive if ≥20% drop in FEV₁.
- FeNO (Fractional exhaled nitric oxide): elevated (>40 ppb) suggests eosinophilic inflammation.
- Allergy testing: skin prick or specific IgE for allergen identification.
- CXR: usually normal, done to rule out other causes.
Treatment (based on GINA 2025 guidelines)
Management aims to control symptoms, prevent exacerbations, and maintain normal lung function.
1. General Principles
- Patient education: trigger avoidance, inhaler technique, adherence.
- Stepwise therapy, adjusted based on control level.
- All adults and adolescents should have ICS-containing therapy (no SABA-only regimen anymore).
2. Stepwise Pharmacological Treatment
Step 1–2 (Mild asthma):
- As-needed low-dose ICS–formoterol (preferred).
- Alternative: daily low-dose ICS + as-needed SABA.
Step 3 (Moderate asthma):
- Low-dose ICS–formoterol maintenance and reliever therapy (MART)
- Alternative: low-dose ICS–LABA + as-needed SABA.
Step 4 (Severe persistent):
- Medium-dose ICS–formoterol MART
- Or medium/high-dose ICS–LABA + SABA as needed.
Step 5:
- Refer for specialist assessment.
- Add-on options:
- LAMA (tiotropium)
- Biologic therapy (e.g., anti-IgE [omalizumab], anti-IL5, anti-IL4R).
- Consider low-dose oral corticosteroids only if unavoidable.
- Add-on options:
3. Acute Exacerbation Management
- Assess severity: speech difficulty, RR, HR, O₂ saturation, PEF.
- Treatment:
- Oxygen to keep SpO₂ 93–95%.
- SABA (salbutamol) via nebulizer or MDI with spacer.
- Add ipratropium bromide if severe.
- Systemic corticosteroids (prednisolone 40–50 mg/day for 5–7 days).
- IV magnesium sulfate in life-threatening or refractory cases.
- Monitor response and admit if poor improvement or previous severe attacks.
Follow-up and Monitoring
- Review control every 1–3 months.
- Step up or down therapy based on symptoms, PEF, and exacerbation frequency.
- Check inhaler technique and adherence before stepping up.
- Vaccinations (influenza, pneumococcal) and smoking cessation are essential.