Ulcerative colitis is a medical issue that affects 6 million cases worldwide. Today we go over everything you’d need to tackle this IBD as a med student.
Ulcerative Colitis
Clinical Picture
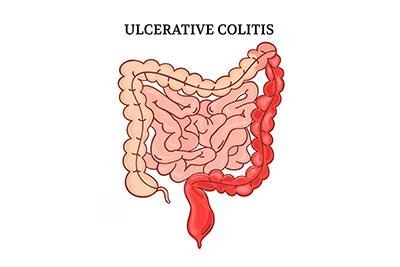
Ulcerative colitis is a chronic inflammatory disease limited to the colon, starting in the rectum and extending proximally in a continuous manner.
Typical presentation includes:
- Bloody diarrhea (most consistent feature)
- Urgency, tenesmus, and lower abdominal cramping
- Mucus in stool
- In severe cases: fever, tachycardia, anemia, weight loss
Extraintestinal manifestations may involve the joints (arthritis), skin (erythema nodosum, pyoderma gangrenosum), eyes (uveitis), and hepatobiliary system (PSC).
Diagnosis
Diagnosis is clinical + endoscopic + histologic.
There’s no single definitive test — UC is diagnosed after excluding infections and Crohn’s disease.
Key steps:
- Laboratory tests:
- CBC (anemia, leukocytosis)
- CRP/ESR (inflammatory activity)
- Electrolytes, albumin (disease severity)
- Stool cultures and C. difficile toxin to exclude infection
- Endoscopy:
- Colonoscopy with biopsies from multiple sites is diagnostic.
- Findings: continuous, circumferential mucosal inflammation starting from the rectum, with loss of vascular pattern, granularity, friability, and ulceration.
- Histopathology:
- Crypt abscesses, glandular distortion, mucosal/submucosal inflammation limited to the mucosa (unlike Crohn’s which is transmural).
- Imaging:
- CT or MR enterography if perforation, toxic megacolon, or Crohn’s overlap is suspected.
Treatment
1. Induction of Remission
- Mild to Moderate (left-sided or proctitis):
- Topical 5-ASA (mesalamine suppository or enema) first-line.
- Add oral 5-ASA if inadequate.
- If refractory → topical corticosteroids or oral budesonide MMX.
- Moderate to Severe:
- Systemic corticosteroids (prednisolone 40–60 mg/day) for induction.
- If steroid-refractory or dependent → escalate to biologic or small-molecule therapy:
- Anti-TNF agents (infliximab, adalimumab, golimumab)
- Anti-integrin (vedolizumab)
- Anti-IL12/23 (ustekinumab)
- JAK inhibitors (tofacitinib, upadacitinib)
- Acute Severe UC (ASUC):
- Admit for IV corticosteroids.
- If no response in 3–5 days → rescue therapy with infliximab or cyclosporine.
- Failure → surgical intervention (colectomy).
2. Maintenance of Remission
- Continue oral ± topical 5-ASA for mild disease.
- For patients induced with biologics or small molecules → continue the same agent for maintenance.
- Avoid long-term steroids.
3. Surgery
- Indications:
- Toxic megacolon or perforation
- Severe refractory disease
- High-grade dysplasia or carcinoma
- Steroid dependence or intolerable side effects
4. Surveillance & Follow-Up
Monitor bone density if on prolonged corticosteroids.
Colorectal cancer screening: Start 8 years after diagnosis; colonoscopy every 1–2 years.
Vaccinations: Ensure hepatitis B, influenza, and pneumococcal vaccines before starting immunosuppressives.
Other Links :